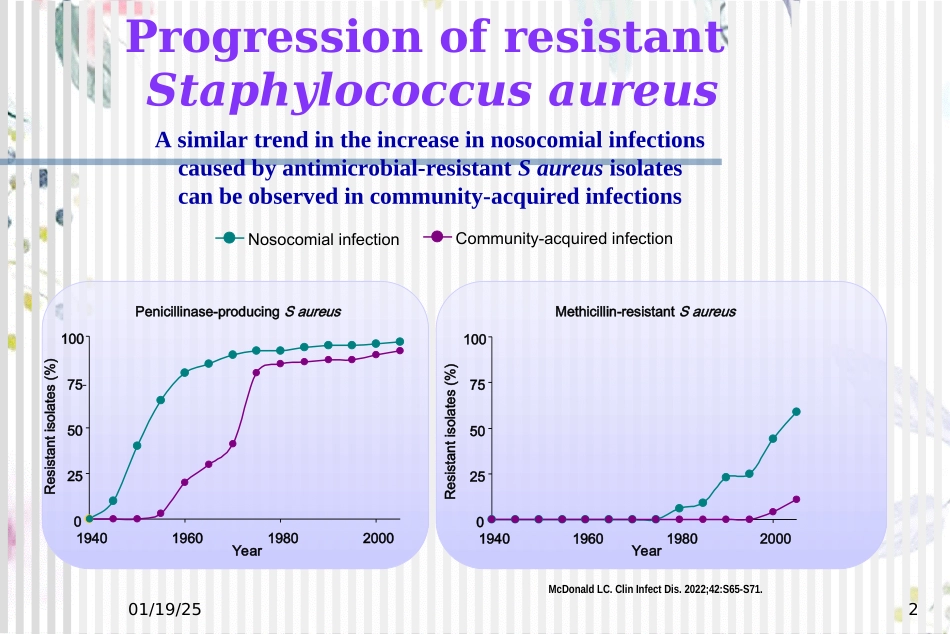
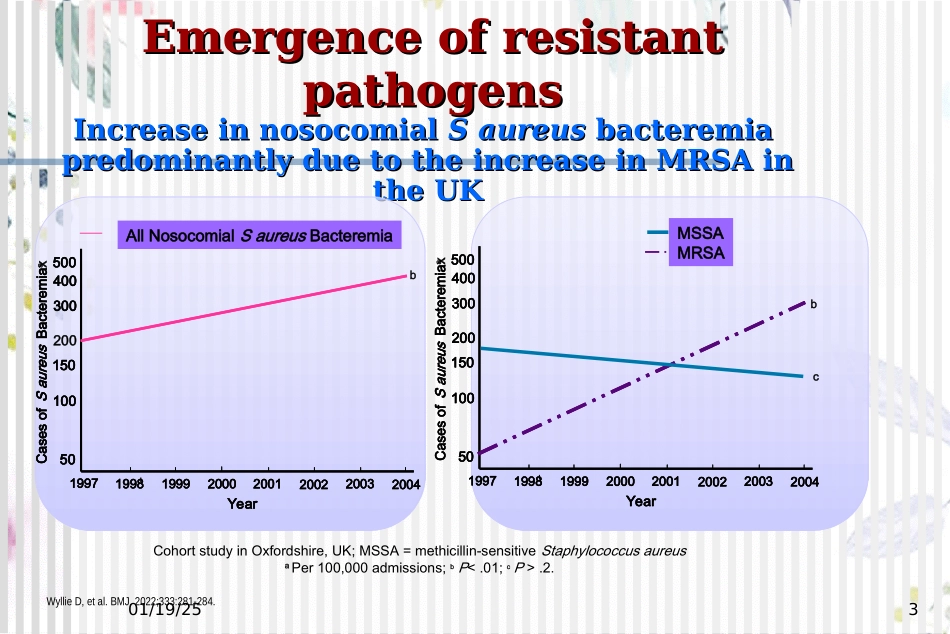
01/19/251MRSA感染的抗菌治疗01/19/252McDonaldLC.ClinInfectDis.2022;42:S65-S71.NosocomialinfectionCommunity-acquiredinfectionPenicillinase-producingSaureus02550751001940196019802000YearResistantisolates(%)Methicillin-resistantSaureus02550751001940196019802000YearResistantisolates(%)ProgressionofresistantStaphylococcusaureusAsimilartrendintheincreaseinnosocomialinfectionscausedbyantimicrobial-resistantSaureusisolatescanbeobservedincommunity-acquiredinfections01/19/253EmergenceofresistantEmergenceofresistantpathogenspathogensIncreaseinnosocomialIncreaseinnosocomialSaureusSaureusbacteremiabacteremiapredominantlyduetotheincreaseinMRSAinpredominantlyduetotheincr...