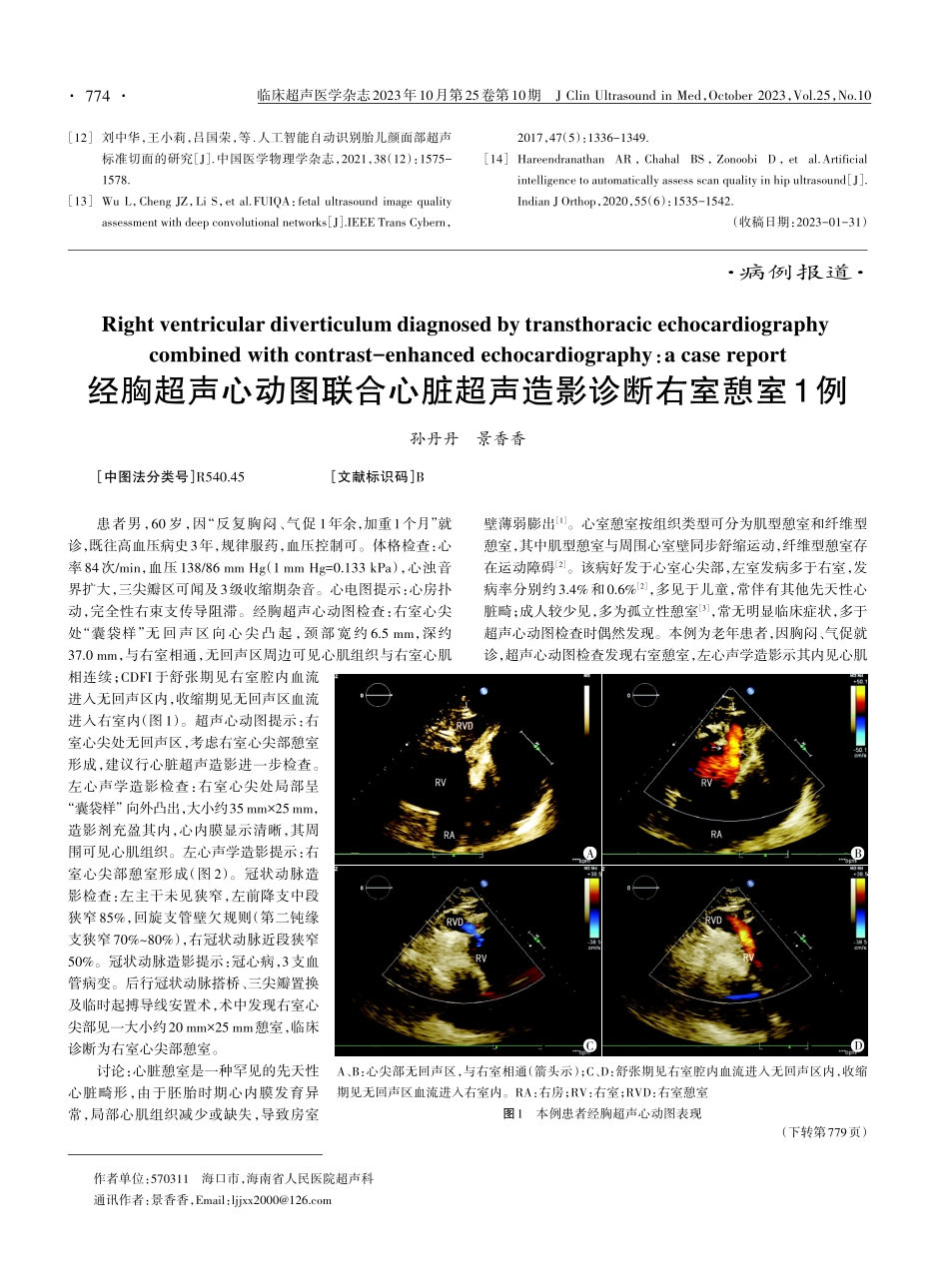
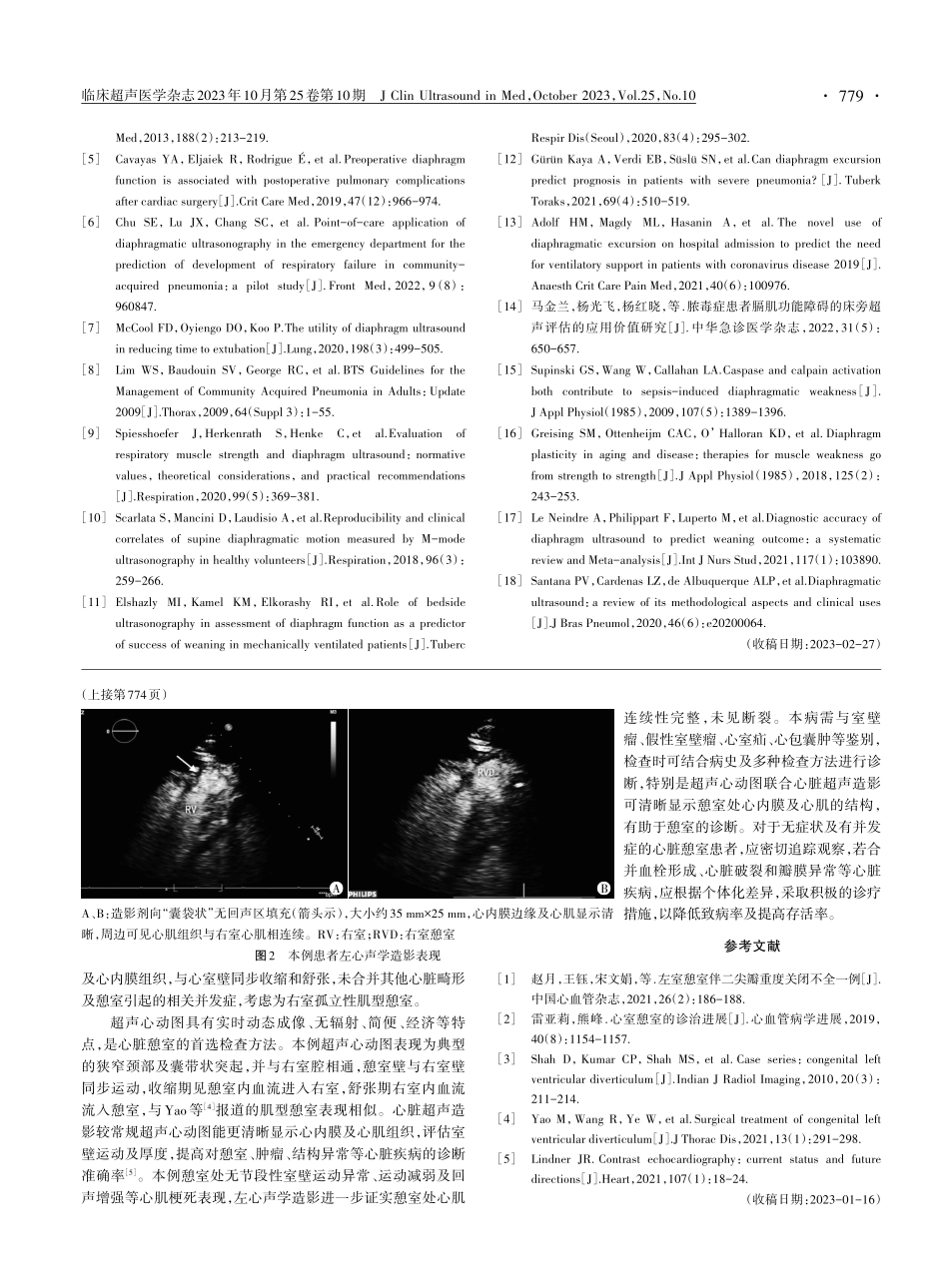
临床超声医学杂志2023年10月第25卷第10期JClinUltrasoundinMed,October2023,Vol.25,No.10[12]刘中华,王小莉,吕国荣,等.人工智能自动识别胎儿颜面部超声标准切面的研究[J].中国医学物理学杂志,2021,38(12):1575-1578.[13]WuL,ChengJZ,LiS,etal.FUIQA:fetalultrasoundimagequalityassessmentwithdeepconvolutionalnetworks[J].IEEETransCybern,2017,47(5):1336-1349.[14]HareendranathanAR,ChahalBS,ZonoobiD,etal.Artificialintelligencetoautomaticallyassessscanqualityinhipultrasound[J].IndianJOrthop,2020,55(6):1535-1542.(收稿日期:2023-01-31)·病例报道·患者男,60岁,因“反复胸闷、气促1年余,加重1个月”就诊,既往高血压病史3年,规律服药,血压控制可。体格检查:心率84次/min,血压138/86mmHg(1mmHg=0.133kPa),心浊音界扩大,三尖瓣区可闻及3级收缩期杂音。心电图提示:心房扑动,完全性右束支传导阻滞。经胸超声心动图检查:右室心尖处“囊袋样”无回声区向心尖凸起,颈部宽约6.5mm,深约37.0mm,与右室相通,无回声区周边可见心肌组织与右室心肌相连续;CDFI于舒张期见右室腔内血流进入无回声区内,收缩期见无回声区血流进入右室内(图1)。超声心动图提示:右室心尖处无回声区,考虑右室心尖部憩室形成,建议行心脏超声造影进一步检查。左心声学造影检查:右室心尖处局部呈“囊袋样”向外凸出,大小约35mm×25mm,造影剂充盈其内,心内膜显示清晰,其周围可见心肌组织。左心声学造影提示:右室心尖部憩室形成(图2)。冠状动脉造影检查:左主干未见狭窄,左前降支中段狭窄85%,回旋支管壁欠规则(第二钝缘支狭窄70%~80%),右冠状动脉近段狭窄50%。冠状动脉造影提示:冠心病,3支血管病变。后行冠状动脉搭桥、三尖瓣置换及临时起搏导线安置术,术中发现右室心尖部见一大小约20mm×25mm憩室,临床诊断为右室心尖部憩室。讨论:心脏憩室是一种罕见的先天性心脏畸形,由于胚胎时期心内膜发育异常,局部心肌组织减少或缺失,导致房室壁薄弱膨出[1]。心室憩室按组织类型可分为肌型憩室和纤维型憩室,其中肌型憩室与周围心室壁同步舒缩运动,纤维型憩室存在运动障碍[2]。该病好发于心室心尖部,左室发病多于右室,发病率分别约3.4%和0.6%[2],多见于儿童,常伴有其他先天性心脏畸;成人较少见,多为孤立性憩室[3],常无明显临床症状,多于超声心动图检查时偶然发现。本例为老...