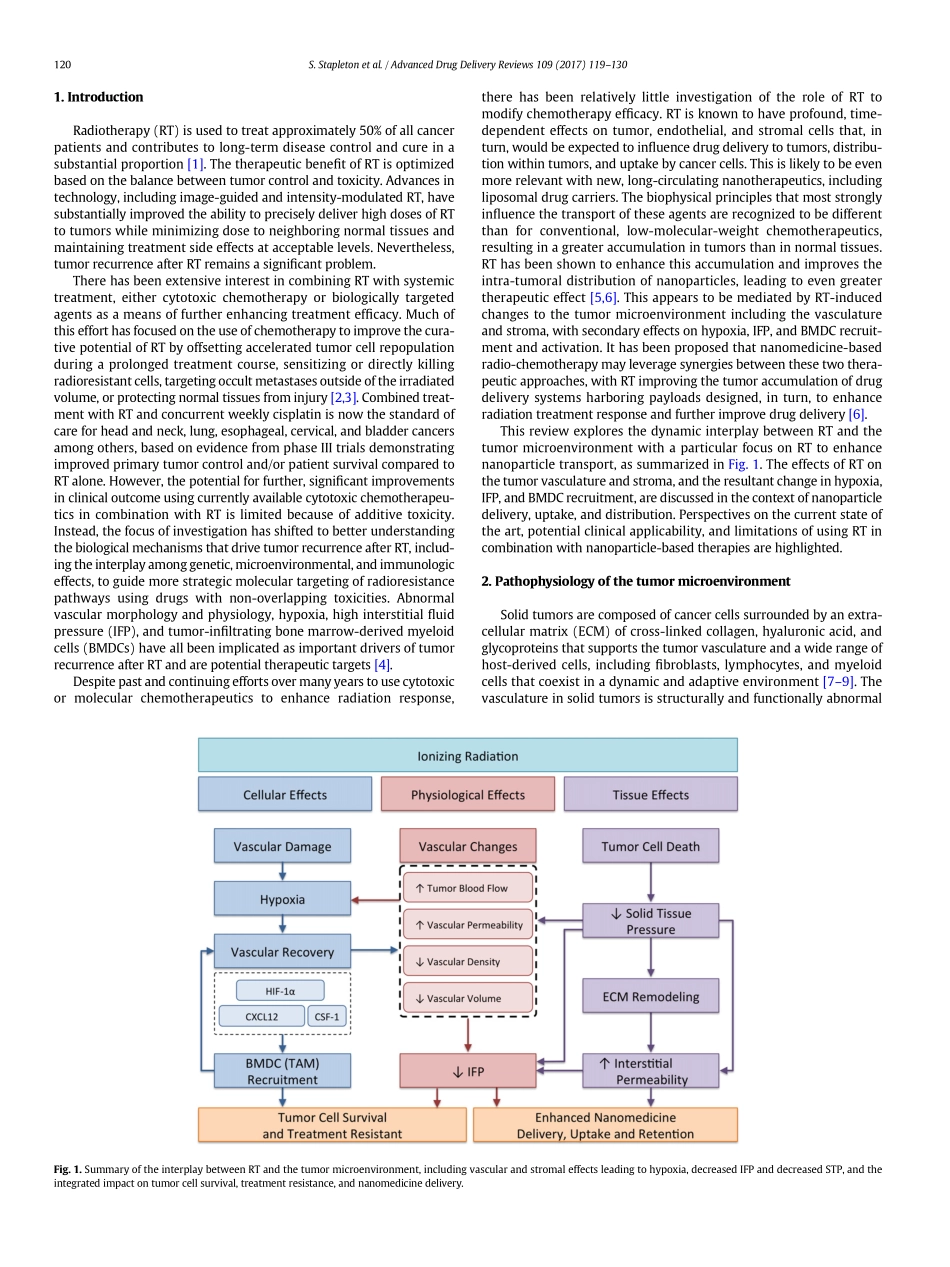
Radiationeffectsonthetumormicroenvironment:Implicationsfornanomedicinedelivery☆ShawnStapletona,DavidJaffraya,b,MichaelMilosevica,b,⁎aRadiationMedicineProgram,PrincessMargaretCancerCentreandUniversityHealthNetwork,Toronto,ON,CanadabDepartmentofRadiationOncology,UniversityofToronto,Toronto,ON,CanadaabstractarticleinfoArticlehistory:Received2December2015Receivedinrevisedform22April2016Accepted24May2016Availableonline1June2016Thetumormicroenvironmenthasanimportantinfluenceoncancerbiologicalandclinicalbehaviorandradiationtreatment(RT)response.However,RTalsoinfluencesthetumormicroenvironmentinacomplexanddynamicmannerthatcaneitherreinforceorinhibitthisresponseandthelikelihoodoflong-termdiseasecontrolinpa-tients.ItisincreasinglyevidentthattheinterplaybetweenRTandthetumormicroenvironmentcanbeexploitedtoenhancetheaccumulationandintra-tumoraldistributionofnanoparticles,mediatedbychangestothevascu-latureandstromawithsecondaryeffectsonhypoxia,interstitialfluidpressure(IFP),solidtissuepressure(STP),andtherecruitmentandactivationofbonemarrow-derivedmyeloidcells(BMDCs).TheuseofRTtomodulatenanoparticledrugdeliveryoffersanexcitingopportunitytoimproveantitumorefficacy.ThisreviewexplorestheinterplaybetweenRTandthetumormicroenvironment,andtheintegratedeffectsonnanoparticledrugdeliveryandefficacy.©2016ElsevierB.V.Allrightsreserved.Keywords:RadiotherapyNanomedicineNanoparticlesTumormicroenvironmentInterstitialfluidpressure(IFP)Tumor-associatedmacrophages(TAMs)DrugtransportEnhancedpermeabilityandretention(EPR)effectContents1.Introduction..............................................................1202.Pathophysiologyofthetumormicroenvironment.............................................1202.1.Tumorhypoxia.........................................................1212.2.Interstitialfluidpressure(IFP)andsolidtissuepressure(STP)....................................1212.3.Bonemarrow-derivedmyeloidcells(BMDCs)...........................................1223.Radiationeffectsonthetumormicroenv...