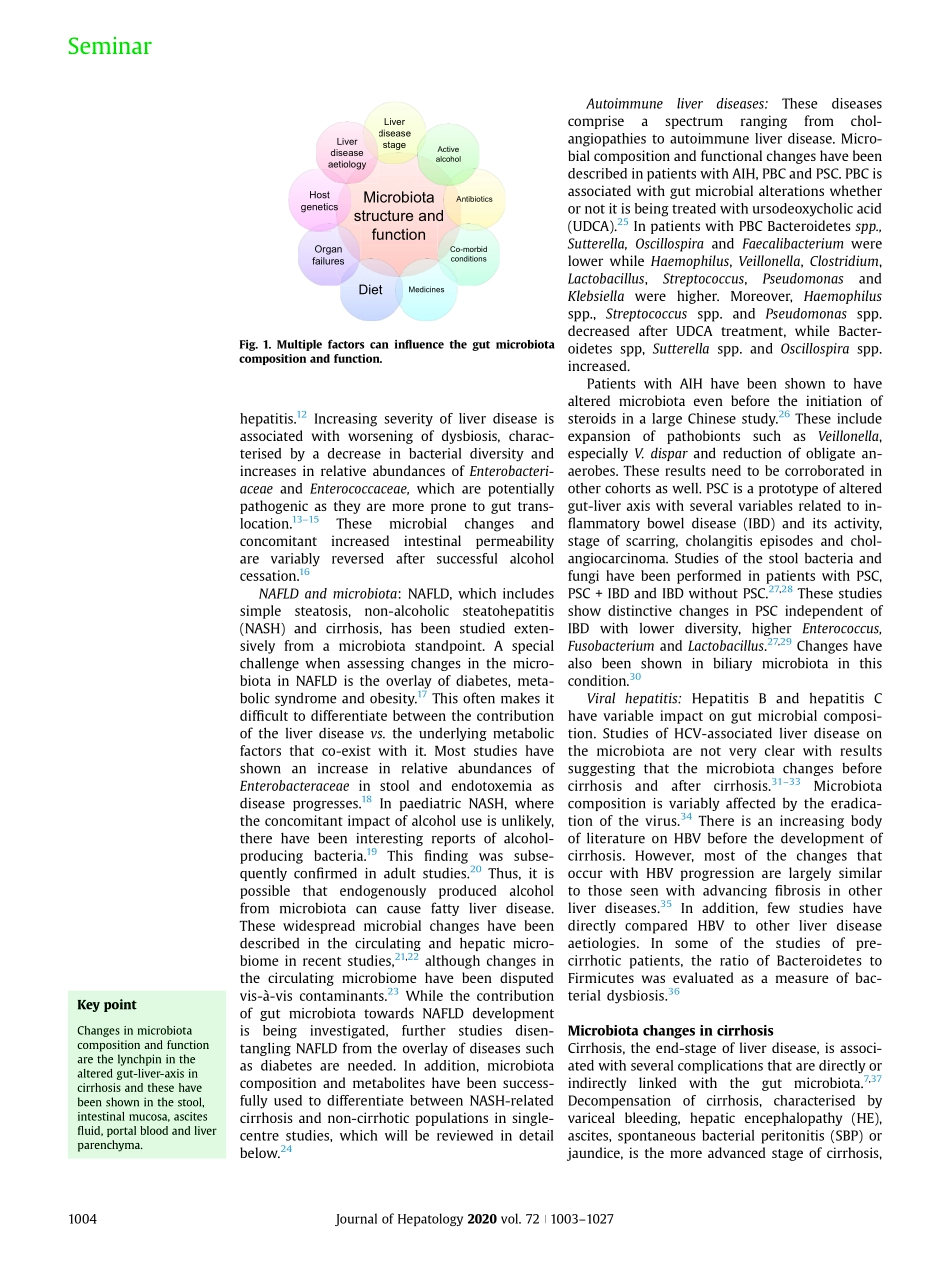
SummaryPatientswithchronicliverdiseaseandcirrhosisdemonstrateaglobalmucosalimmuneimpairment,whichisassociatedwithalteredgutmicrobiotacompositionandfunctionality.Thesechangesprogressalongwiththeadvancingdegreeofcirrhosisandcanbelinkedwithhepaticencephalopathy,infectionsandevenprognosticationindependentofclinicalbiomarkers.Alongwithcompositionalchanges,func-tionalalterationstothemicrobiota,relatedtoshort-chainfattyacids,bioenergeticsandbileacidmetabolism,arealsoassociatedwithcirrhosisprogressionandoutcomes.Alteringthefunctionalandstructuralprofileofthemicrobiotaispartlyachievedbymedicationsusedinpatientswithcirrhosissuchasrifaximin,lactulose,protonpumpinhibitorsandotherantibiotics.However,theroleoffaecalorin-testinalmicrobiotatransplantationisincreasinglybeingrecognised.Herein,wereviewthechallenges,opportunitiesandroadaheadfortheappropriateandsafeuseofintestinalmicrobiotatransplantationinliverdisease.©2020EuropeanAssociationfortheStudyoftheLiver.PublishedbyElsevierB.V.Allrightsreserved.IntroductionChangesinthecompositionandfunctionalityofintestinalmicrobiotacontributetotheprogressionofchronicliverdiseaseandmakeanattractivetargetforintervention.1,2Whilevariousintrinsicandextrinsicfactors,suchasethnicity,age,diet,co-morbidconditionsandmedicationsaffecttheintestinalmicrobiota(Fig.1),3furtheruniqueco-variates,suchasalcohol,diseaseaetiology,stageofliverdisease,andthemultiplemicrobiota-modifyingmedicationsneedtobeconsideredinthesepa-tients.4Inaddition,itisimportanttorememberthatmostliverdiseasesarelifestyle-relatedandthera-piestargetingthemicrobiotarepresentonlyoneaspectofthemulti-prongedinterventionalapproachthatisneededinthesepatients.4–6Oflate,faecalorintestinalmicrobiotatrans-plantationorFMT/IMThasbeenincreasinglyusedinchronicliverdisease.7ThisreviewwillfocusonmicrobiotachangesinhumanpatientswithchronicliverdiseaseandthecurrentandfutureFMT/IMTstudiesinthispopulation.WewilldiscussFMT/IMTfromapharmacologicalperspectiveandrefertothetreatmentstrategyas‘IMT’,asrecentl...