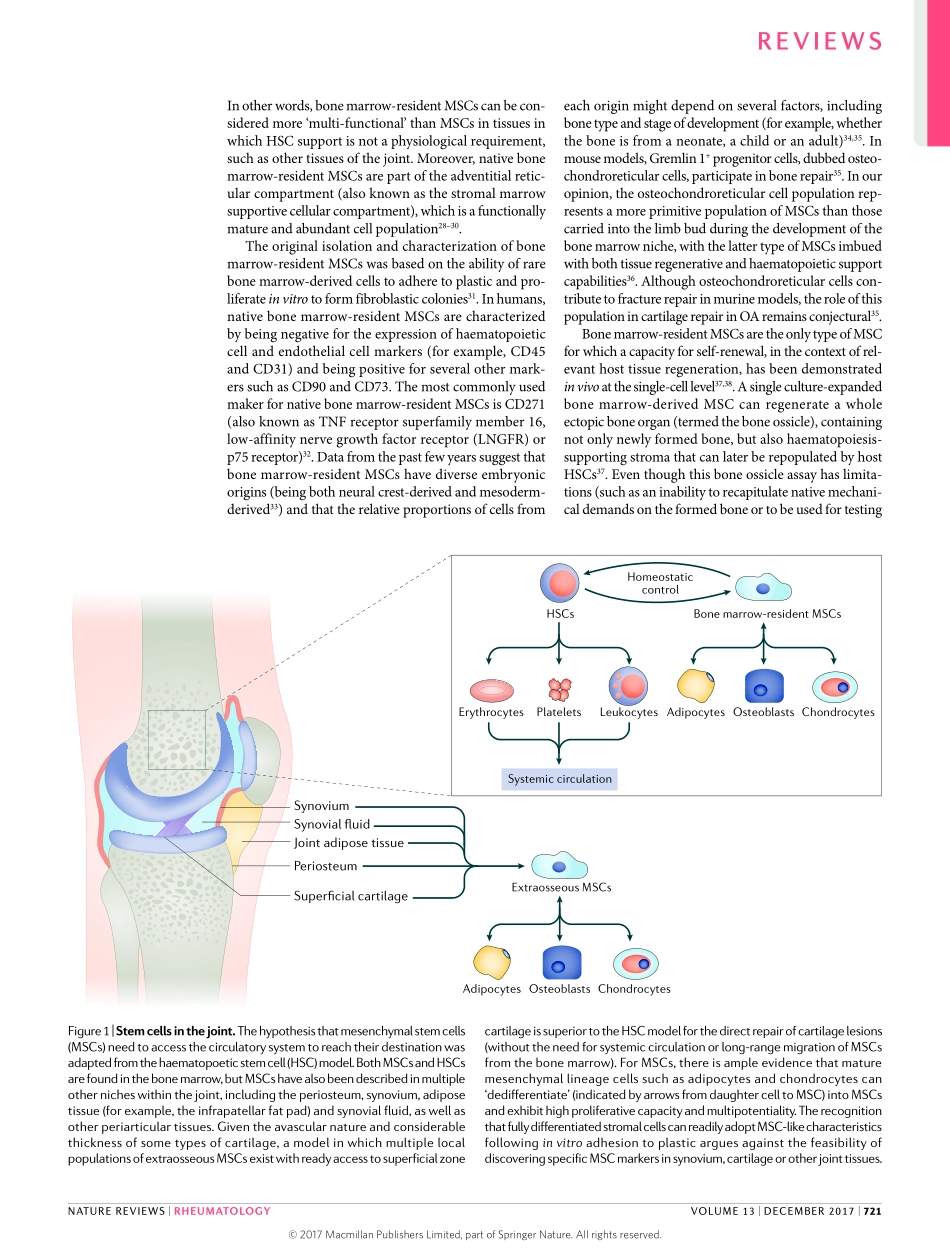
Thepathogenesisofosteoarthritis(OA)iscomplexandheterogeneous,withbothdiseaseinitiationandprogres-sionbeingdependentonmultiplejointstructures,includ-ingcartilage,bone,ligaments,meniscusandsynovium1,2.Manyresearcharticlesandreviewshaveemphasizedtheroleofculture-expandedcellulartherapies,scaffoldsanddrugsinthedevelopmentoftherapiesforOA,especiallyfor‘chondrogenic’OA,butthereisapaucityofdataontheuseofnative(notculture-expanded)joint-residentstemcellsinjoint-repairstrategies.ThisReviewwillfocuson‘chondrogenic’OA,inwhichdiseaseinitiationandprogressionseemtobecriticallydependentonthearticularcartilage.Theroleofsubchondralbone,includ-ingtheosteochondraljunction,isalsoimportantinthepathogenesisofOAandhasbeendiscussedextensivelyelsewhere3;therefore,ourcommentsonthissubjectwilllargelyfocustotheroleofnativebonemarrow-residentstemcells,especiallyatsitesofcartilagedenudationinadvancedOA,wheresuchtopographicallylocalizedcellscandirectlyaccessthejointcavity.ThepivotalroleofarticularcartilagelossinOA4,5andtherecognitionthatcartilagecanberestored,albeitwithrelativelypoor-qualityrepairtissue,followingmicro-fracturetechniquesinpatientswithisolatedcartilagelesionsorfollowingautologouschondrocyteimplanta-tionforthetreatmentoffull-thicknesslesions6,7,pointedtothepotentialimportanceofcartilageinthedevelop-mentoftherapiesforOA.Theseearlystudies6,7suggestedthatcartilagerepaircouldoccurviatheactionsofhighlyproliferativecellsincloseproximitytothecartilage,andwereakeyimpetusforthesubsequentcultureexpansioncellularprotocols(firstpopularisedinthe1990s6)andforthesubsequentjoint-repairstrategiesthatusedcombina-tionsofculture-expandedcellsandadjuncts,includingscaffoldsandpharmaceuticalagents8.AlthoughitmightnotbepossibletoextrapolatethepotentialbenefitsofcellulartherapyfromresultsinisolatedcartilagedefectsinyoungindividualstodefectsinpatientswithadvancedOA,thereisevidencethatisolatedcartilagelesionsinskeletallymatureindividualsincreaseinseverityovertime9–11,suggestingthatadvancesinthetreatme...