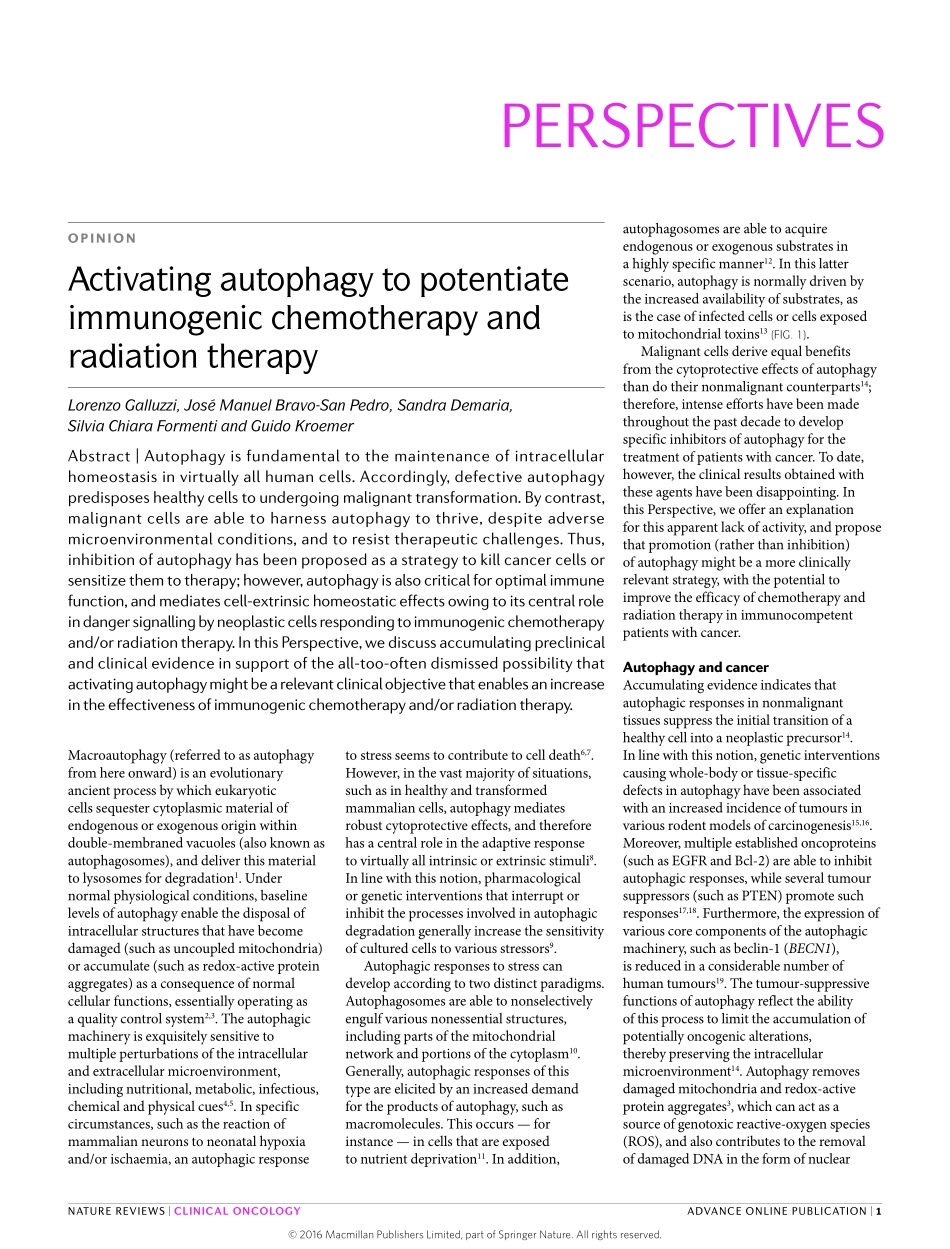
Macroautophagy(referredtoasautophagyfromhereonward)isanevolutionaryancientprocessbywhicheukaryoticcellssequestercytoplasmicmaterialofendogenousorexogenousoriginwithindouble-membranedvacuoles(alsoknownasautophagosomes),anddeliverthismaterialtolysosomesfordegradation1.Undernormalphysiologicalconditions,baselinelevelsofautophagyenablethedisposalofintracellularstructuresthathavebecomedamaged(suchasuncoupledmitochondria)oraccumulate(suchasredox-activeproteinaggregates)asaconsequenceofnormalcellularfunctions,essentiallyoperatingasaqualitycontrolsystem2,3.Theautophagicmachineryisexquisitelysensitivetomultipleperturbationsoftheintracellularandextracellularmicroenvironment,includingnutritional,metabolic,infectious,chemicalandphysicalcues4,5.Inspecificcircumstances,suchasthereactionofmammalianneuronstoneonatalhypoxiaand/orischaemia,anautophagicresponseautophagosomesareabletoacquireendogenousorexogenoussubstratesinahighlyspecificmanner12.Inthislatterscenario,autophagyisnormallydrivenbytheincreasedavailabilityofsubstrates,asisthecaseofinfectedcellsorcellsexposedtomitochondrialtoxins13(FIG.1).Malignantcellsderiveequalbenefitsfromthecytoprotectiveeffectsofautophagythandotheirnonmalignantcounterparts14;therefore,intenseeffortshavebeenmadethroughoutthepastdecadetodevelopspecificinhibitorsofautophagyforthetreatmentofpatientswithcancer.Todate,however,theclinicalresultsobtainedwiththeseagentshavebeendisappointing.InthisPerspective,weofferanexplanationforthisapparentlackofactivity,andproposethatpromotion(ratherthaninhibition)ofautophagymightbeamoreclinicallyrelevantstrategy,withthepotentialtoimprovetheefficacyofchemotherapyandradiationtherapyinimmunocompetentpatientswithcancer.AutophagyandcancerAccumulatingevidenceindicatesthatautophagicresponsesinnonmalignanttissuessuppresstheinitialtransitionofahealthycellintoaneoplasticprecursor14.Inlinewiththisnotion,geneticinterventionscausingwhole-bodyortissue-specificdefectsinautophagyhavebeenassociatedwithanincreasedincidenceoftumoursinvario...