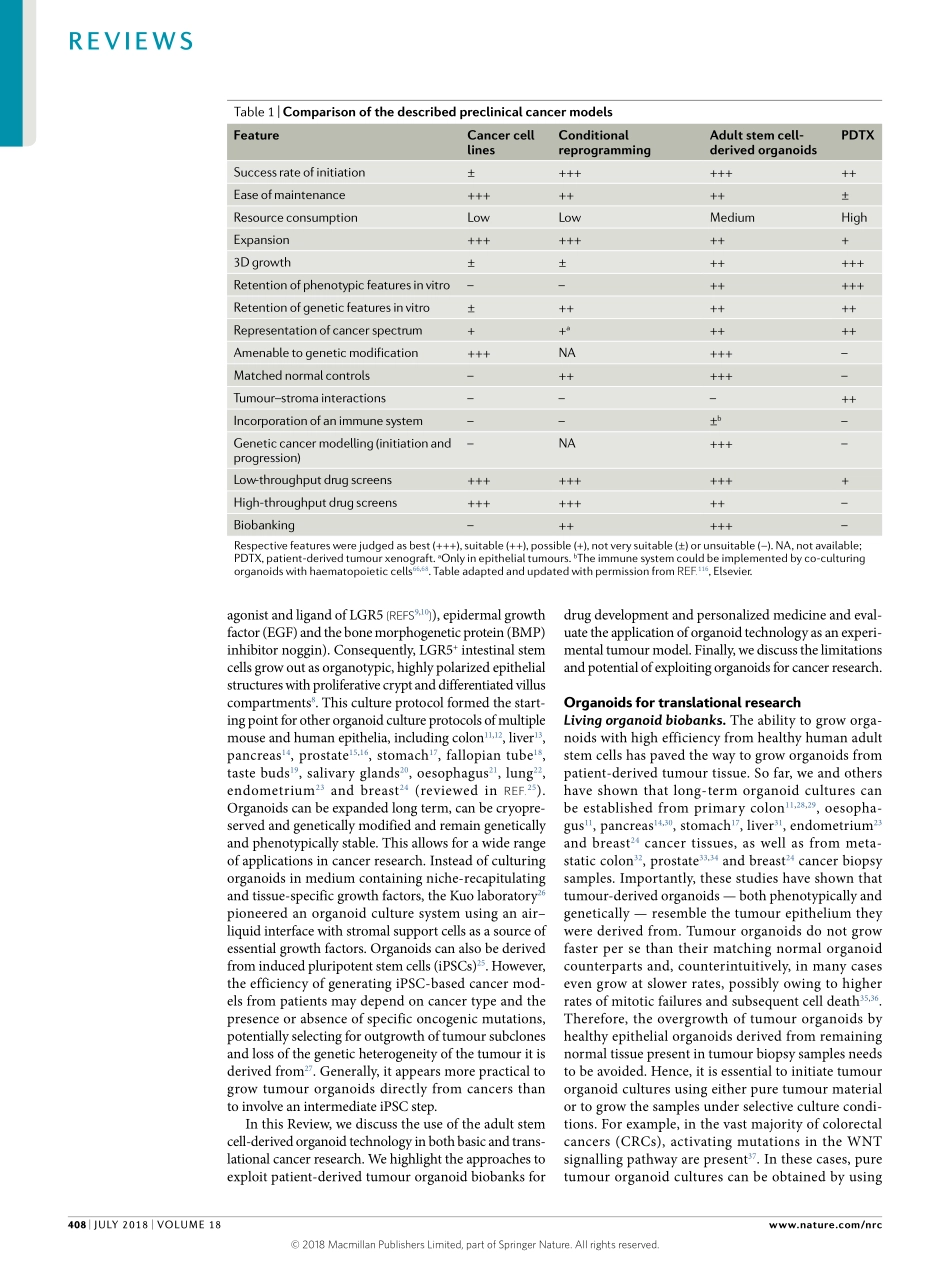
Overthepastdecades,ourknowledgeoftheoriginofcancerhasincreasedimmensely.Despitesubstantialprogressinthetreatmentof(certaintypesof)cancer,itremainsamajorworldwidehealthproblem1.Thenumberofcancerdeathsmaybereducedbypreven-tivemeasurementsandearlydetection.Inaddition,thedevelopmentofnew,moretargetedtherapiesoffersopportunities.Oneofthemajorhurdlesforthedevel-opmentofnoveltreatmentregimensisthechallengeoftranslatingscientificknowledgefrombenchtobedside,whichismainlyduetothefactthatmanycancermodelsonlypoorlyrecapitulatethepatient’stumour2,andasaconsequence,manydrugsthatperformwellincancermodelsultimatelyfailinclinicaltrials3.Althoughanimalcancermodelshaveprovidedimportantinsightsintothebasicsofcancer,theirgenerationistimeconsuming,anditisarguedthatthesemodelsoftendonotfaithfullyreca-pitulatepathogenicprocessesinpatients.Forexample,thehistologicalcomplexityandgeneticheterogeneityofhumancancersaretypicallynotreflectedingeneticallyengineeredmousemodelsofcancer4.Commonlyusedhumancancermodelsincludecancercelllinesandprimarypatient-derivedtumourxenografts(PDTXs).Cancercelllinesarederivedfromprimarypatientmaterialandhavecontributedtremen-douslytocancerresearch.However,theyhaveseveraldrawbacks.Forinstance,theirgenerationfromprimarypatientmaterialisveryinefficientandinvolvesextensiveadaptationandselectiontoinvitro2Dculturecondi-tions.Asonlyrareclonesareabletoexpandandcanbemaintainedovermanypassages,thederivedcelllinesmayhaveundergonesubstantialgeneticchangesandnolongerrecapitulatethegeneticheterogeneityoftheoriginaltumours.Otherlimitationsofcelllinesincludetheabsenceofnormaltissue-derivedcontrolcelllinesasreferenceandthelackofstromalcompartments(Table1).Arecentlydevelopedmethodcalled‘condi-tionalreprogramming’facilitatestheestablishmentof2Dcellculturesfromnormalandtumourepithelialcellswithhighefficiency5.Theseculturescanbemain-tainedlongtermandretainastablekaryotype.Thepro-cedureinvolvesthepresenceofaRHOkinaseinhibitorandfibroblastfeedercells5(Table1).PDTXshavetheadvantageo...