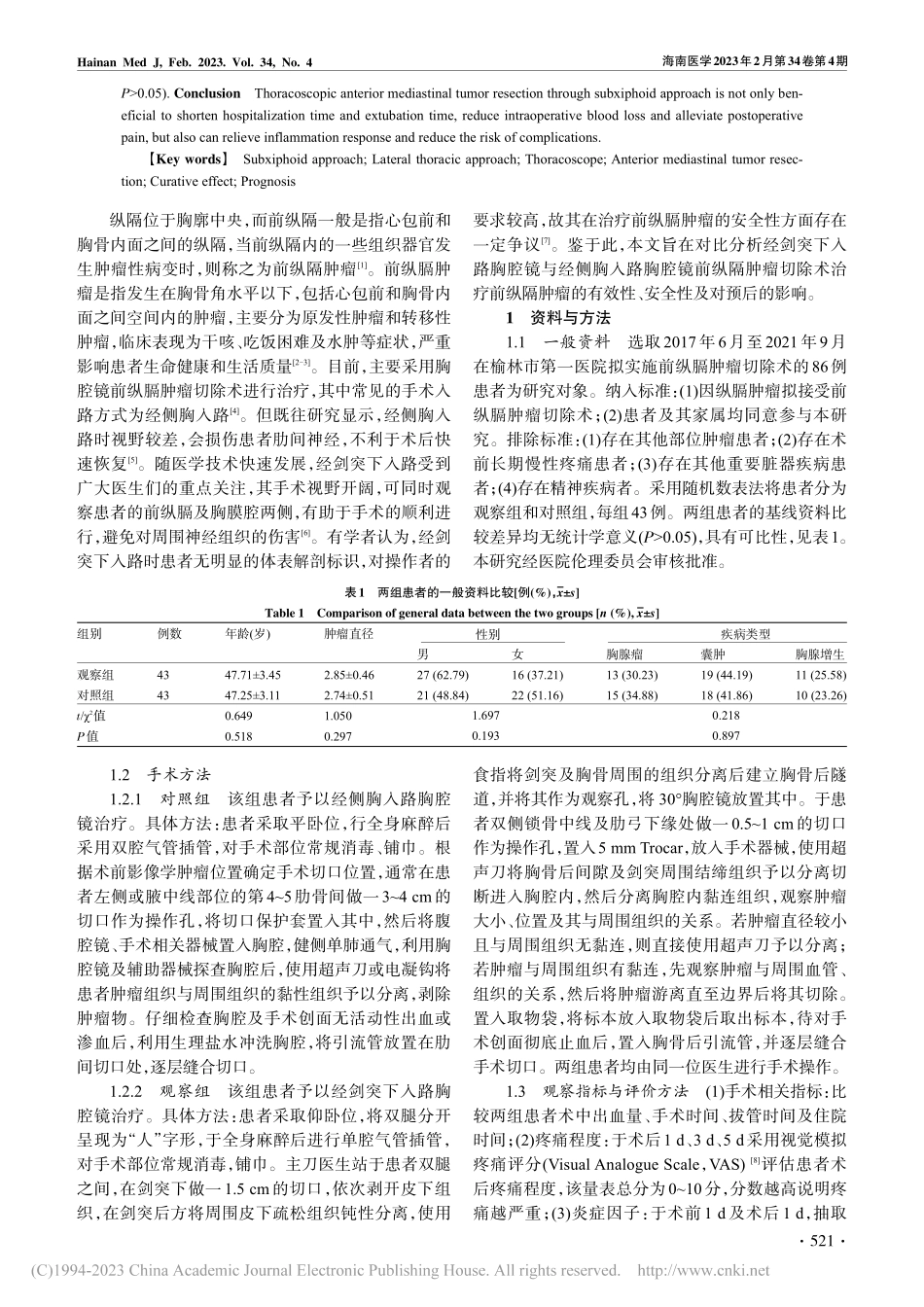
海南医学2023年2月第34卷第4期HainanMedJ,Feb.2023.Vol.34,No.4不同入路胸腔镜手术治疗前纵隔肿瘤的临床疗效对比研究刘鹏,郝登荣,彭彦才,席俊峰,张志斌,李伟伟榆林市第一医院胸心外科,陕西榆林719000【摘要】目的比较经剑突下入路胸腔镜与经侧胸入路胸腔镜前纵隔肿瘤切除术的临床治疗效果。方法选取2017年6月至2021年9月在榆林市第一医院拟实施前纵膈肿瘤切除术的患者86例,采用随机数表法分为观察组和对照组各43例。对照组患者予以经侧胸入路胸腔镜治疗,观察组患者予以经剑突下入路胸腔镜治疗。比较两组患者的手术相关指标(术中出血量、手术时间、拔管时间及住院时间);于手术前后,比较患者的炎症因子水平[血清C-反应蛋白(CRP)、白细胞(WBC)和中性粒细胞比例];采用视觉模拟疼痛评分(VAS)评价两组患者术后不同时间的疼痛程度并记录两组患者的并发症发生情况;于术后随访6个月比较两组患者的复发率。结果观察组患者的术中出血量、拔管时间、住院时间分别为(63.47±7.22)mL、(3.49±1.03)d、(7.35±1.24)d,明显少(短)于对照组的(76.39±7.52)mL、(4.86±1.09)d、(9.57±1.37)d,差异均具有统计学意义(P<0.05);观察组患者术后1d、3d、5d的VAS评分分别为(2.54±0.87)分、(2.01±0.50)分、(1.37±0.31)分,明显低于对照组的(3.22±1.03)分、(2.95±0.62)分、(2.28±0.59)分,差异均有统计学意义(P<0.05);术后,观察组患者的CRP、WBC及中性粒细胞比例分别为(8.16±1.82)mg/L、(8.52±1.36)×109/L、(61.25±5.33)%,明显低于对照组的(10.89±1.91)mg/L、(10.43±1.50)×109/L、(70.13±5.40)%,差异均具有统计学意义(P<0.05);观察组患者的并发症发生率为6.98%,明显低于对照组的23.26%,差异均具有统计学意义(P<0.05);观察组患者术后6个月的复发率为2.33%,略低于对照组的6.98%,但差异无统计学意义(P>0.05)。结论经剑突下入路胸腔镜用于前纵隔肿瘤切除术,不仅有助于缩短患者住院时间、拔管时间,降低术中出血量、术后疼痛程度,而且能减轻炎症反应及减少并发症发生风险。【关键词】经剑突下入路;经侧胸入路;胸腔镜;前纵隔肿瘤切除术;疗效;预后【中图分类号】R738【文献标识码】A【文章编号】1003—6350(2023)04—0520—05Comparativestudyontheclinicalcurativeeffectofthoracoscopicsurgerythroughdifferentapproachesonanteriormediastinaltumor.LIUPeng,HAODeng-rong,PENGYan-cai,XIJun-feng,ZHANGZhi-bin,LIWei-wei.Departmen...