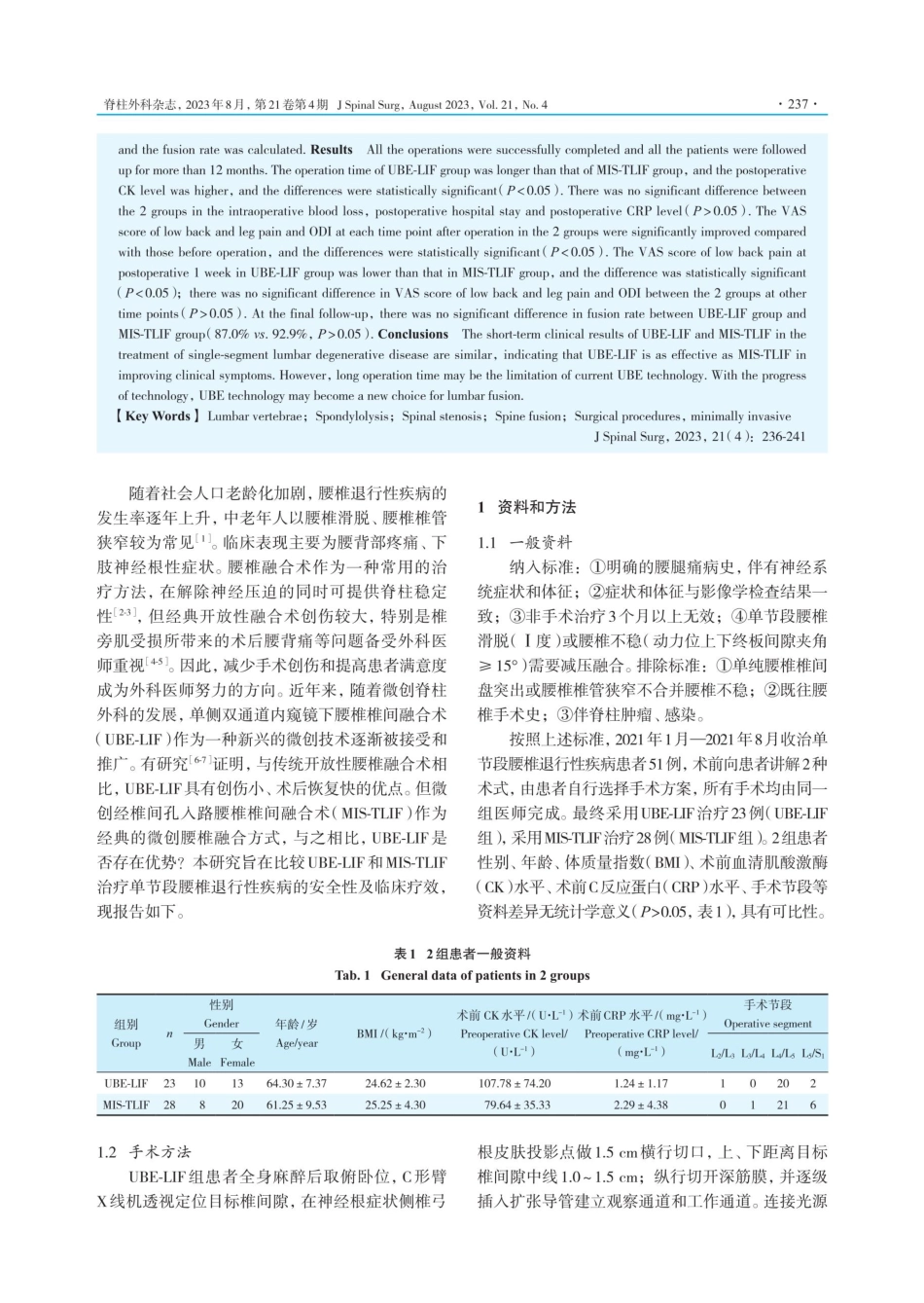
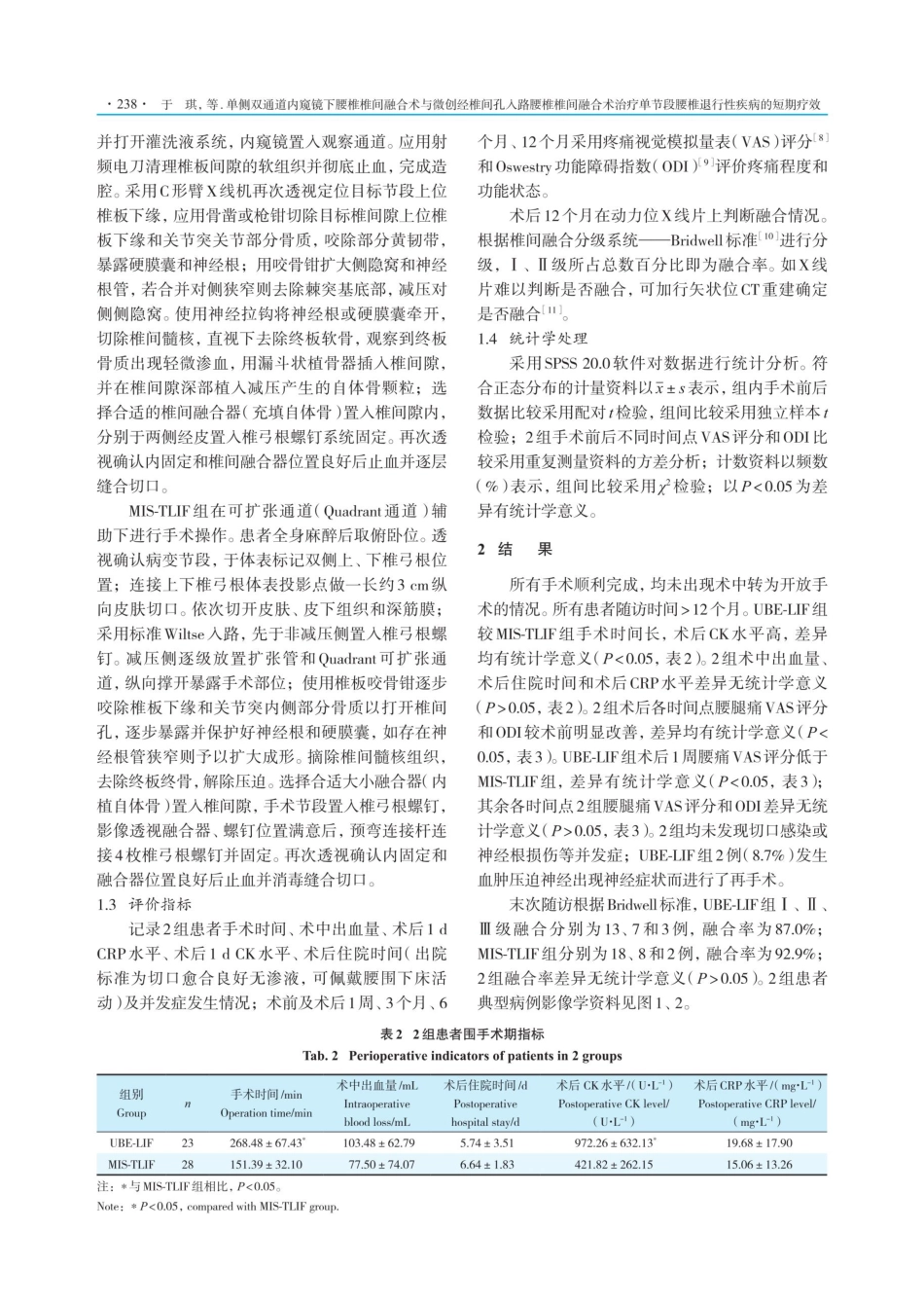
·236·于琪,等.单侧双通道内窥镜下腰椎椎间融合术与微创经椎间孔入路腰椎椎间融合术治疗单节段腰椎退行性疾病的短期疗效·临床研究·单侧双通道内窥镜下腰椎椎间融合术与微创经椎间孔入路腰椎椎间融合术治疗单节段腰椎退行性疾病的短期疗效于琪12,胡旭琪²,潘学康²,张建乔3,陆惠根1,21.蚌埠医学院研究生院,蚌埠2330302.嘉兴学院附属第二医院骨科,嘉兴3140013.浙江中医药大学附属嘉兴市中医院骨科,嘉兴314015【摘要】目的比较单侧双通道内窥镜下腰椎椎间融合术(UBE-LIF)和微创经椎间孔人路腰椎椎间融合术(MIS-TLIF)治疗单节段腰椎退行性疾病的早期临床疗效和影像学结果。方法2021年1月一2021年8月嘉兴学院附属第二医院收治单节段腰椎退行性疾病患者51例,其中23例采用UBE-LIF治疗(UBE-LIF组),28例采用MIS-TLIF治疗(MIS-TLIF组)。记录2组患者手术时间、术中出血量、术后1dC反应蛋白(CRP)水平、术后1d血清肌酸激酶(CK)水平、术后住院时间及并发症发生情况;术前及术后1周、3个月、6个月、12个月采用疼痛视觉模拟量表(VAS)评分和Oswestry功能障碍指数(ODI)评价疼痛程度和功能状态;末次随访时观察融合情况并计算融合率。结果所有手术顺利完成,所有患者随访时间>12个月。UBE-LIF组较MIS-TLIF组手术时间长,术后CK水平高,差异均有统计学意义(P<0.05)。2组术中出血量、术后住院时间和术后CRP水平差异无统计学意义(P>0.05)。2组术后各时间点腰腿痛VAS评分和ODI较术前明显改善,差异均有统计学意义(P<0.05)。UBE-LIF组术后1周腰痛VAS评分低于MIS-TLIF组,差异有统计学意义(P<0.05);其余各时间点2组腰腿痛VAS评分和ODI差异无统计学意义(P>0.05)。末次随访时,UBE-LIF组(87.0%)和MIS-TLIF组(92.9%)融合率差异无统计学意义(P>0.05)。结论UBE-LIF和MIS-TLIF治疗单节段腰椎退行性疾病术后短期临床疗效相似,表明UBE-LIF在改善临床症状方面与MIS-TLIF同样有效。然而,较长的手术时间可能是当前UBE技术的局限性,随着技术的进步,UBE技术可能成为腰椎融合术的新选择。【关键词】腰椎;脊椎滑脱;椎管狭窄;脊柱融合术;外科手术,微创性【中图分类号】R681.533【D01】10.3969/jissn.1672-2957.2023.04.005Short-termeffectofunilateralbiportalendoscopiclumbarinterbodyfusionandminimallyinvasivetransforaminallumbarinterbodyfusiononsingle-segmentlumbardegenerativediseaseYuQil.2,HuXuqie,PanXuekang,ZhangJian...