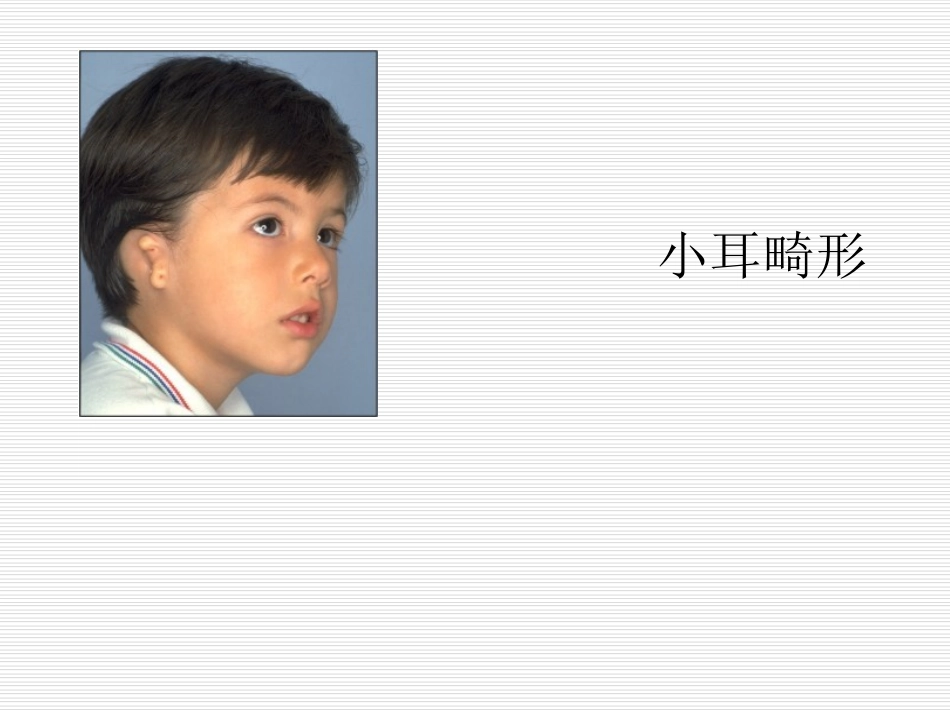
小耳畸形TheNagataTechnique•BackgroundFirstintroducedin1993,theNagatatechniquehasenjoyedwidesuccessasanalternativetotheBrenttechnique.Itsmajoradvantageliesinitstwo-stagedapproach•ThefirststageoftheNagatatechniqueinvolves:1.Fabricationandinsertionofacartilageframework2.TranspositionofthelobuleThisroughlycorrespondstothefirstthreestagesoftheBrenttechniqueFirstStageUsetheipsilateral6th–9thcostalcartilagesinfabricatingtheframeworkHarvestingofthecostalcartilages•Theframeworkisconstructedinthreedistinctlevelsor“floors”1.Firstfloor:thecrushelicis、fossatriangularis2.Secondfloor:thescapha3.Thirdfloor:thehelix、antihelix、tragus,antitragusFabrication–The6t...